Dealing with Winter Depression: 6 Questions about Seasonal Affective Disorder
 To answer key questions about Seasonal Affective Disorder, FoundHealth sat down with Amy J. Ahlfeld, Psy.D., a Clinical Psychologist based out of Sacramento, California. She is the current President of the Sacramento Valley Psychological Association and maintains a private practice specializing in working with individuals and couples on parenting, women’s issues, relationship violence, anger management and gambling addiction. She has been practicing for 8 years.
To answer key questions about Seasonal Affective Disorder, FoundHealth sat down with Amy J. Ahlfeld, Psy.D., a Clinical Psychologist based out of Sacramento, California. She is the current President of the Sacramento Valley Psychological Association and maintains a private practice specializing in working with individuals and couples on parenting, women’s issues, relationship violence, anger management and gambling addiction. She has been practicing for 8 years.
Introduction to SAD: Seasonal Affective Disorder is a kind of depression that takes effect seasonally, usually during the winter months. Sufferers tend to feel excessive tiredness and have an increase in appetite. Difficulty waking up in the morning, cravings for carbohydrates, lack of energy, withdrawal from friends and family, and decreased sex drive can all be symptoms.
1. What is the difference between Seasonal Affective Disorder and Depression? Are they the same?
Amy: In the spectrum of psychological disorders, SAD disorder and depression are closely related. In fact, SAD isn’t actually recognized as a different disorder, instead it is really just one category of depression. The key distinction is that depressive symptoms that fall under the realm of SAD are occur seasonally, as the name suggests. It tends to affect people in the fall and winter season when days are shorter and there is less sunlight. Symptoms frequently parallel mild depression, with sleep patterns, mood, and general feelings of well-being becoming disrupted.
The main thing to pay attention to recognizing the timing of your symptoms. If an individual is consistently feeling down, the season may not be correlated with those symptoms. However, if a person feels fine during the summer but annually feels depression in winter, that is an indication of SAD disorder, and it should be treated as such.
2. So are both Seasonal Affective Disorder and Depression treated in the same way?
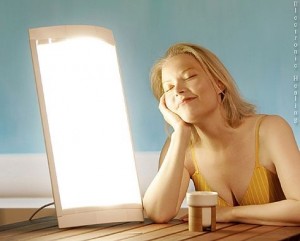
Amy: Not exactly. One of the first line treatment for Seasonal Affective Disorder is light therapy. Research has suggested that the changes in photoperiod – the amount of light per day – causes chemical changes in the brain which consequently spark depressive symptoms. Light therapy attempts to reset a person’s body clock by having a patient sit in front of a light box for a set time frame per day, usually between 30 and 60 minutes. This often triggers the body to correct its chemical imbalances naturally, and can be as effective and cause less side effects than anti-depressants.
When a person is experiencing a severe case of SAD disorder, in addition to light therapy, other empirically based treatments for depression are utilized such as cognitive behavioral therapy, psychotropic medication, etc.
3. What if I just feel mildly depressed during winter, but I don’t think I need to see a doctor. Are there things I can do to help myself get better, asides from medication or light therapy?
Amy says: First of all, take inventory of your physical health. Research demonstrates a direct link between physical health and mental health. For instance, ask yourself if you are exercising. Do you have regular activity in your daily life? There are numerous studies about how exercise is a natural anti-depressant. Endorphins and a good mood follow a good workout and also promotes positive choices regarding food & nutrition and ability to cope with stressors. Physical activity works. Force yourself to adhere to routines that promote positive health practices such as waking up early, getting out of bed, showering daily, getting dressed, eating at least 3 balanced meals, etc. These are called ‘behavioral activation strategies.’
The second strategy is to try not to isolate yourself. Depressed people tend to do that. If you force yourself to confide in others, ask for help, and socialize with family, friends, and/or colleagues, it can really help.
Lastly, make sure you are setting realistic goals. A lot of folks in my practice come in with low-grade depression, and many times it is because they have these huge goals and their life experience does not match these wants/needs. There is a clear disconnect, and thus they feel defeated, discouraged, and depressed. Partly, it is because their goals are unrealistic – ask yourself, do your goals make sense for you right now at this stage of the game? If they don’t, change your goals and/or change your approach to achieving them. It is often helpful to break up the goals into smaller, more achievable goals that can promote more confidence and less distress which can really help with both mild and moderate depression.
4. If I feel like a family member or close friend is exhibiting signs of SAD disorder or depression, what should I do?
Amy says: Offer emotional support, understanding, encouragement and have patience. You must listen and not disparage the emotions that someone is expressing. Don’t ever ignore comments of suicide.
If you are the partner, the loved one, ask the depressed person what he or she needs. It may be helpful to conceptualize yourself as the depressed person’s coach. Suggest doing activities that are physical and if possible, offer to engage in these activities together. You can also help by breaking down unrealistic expectations and/or offering alternative strategies for reaching goals that are attainable. If the symptoms persist, encourage your partner or loved one to see a specialist in the mental health field (psychologist, psychiatrist, or other mental health practitioner).
5. What is the longest a person should wait before seeing a specialist?
There is no uniform answer on the amount of time someone should wait. Certain people, if depressed for a week, will make sure they seek out a specialist right away. Others wait years before seeking out help. The bottom line is that if someone feels like their depressive symptoms are impairing their quality of life or are interfering with their activities of daily functioning, they should absolutely seek treatment as soon as possible.
6. Are their any supplements that you would recommend for dealing with SAD or Depression?
St. John’s Wort is the first that comes to mind. There have been studies that have shown benefit for people who have mild or moderate depression. However, for people who are severely depressed, it does not appear there is solid evidence for improvement. Read more on Depression and St. John’s Wort.
Omega-3 fatty acids have been shown to have an effect. There has been 6 published studies using Omega-3’s for depression, and all of them showed significant improvement when compared to placebo. It seems to interact with neurotransmitters and allows increased serotonin and dopamine transmission. Read more on Depression and Omega-3’s.
Another is SAM-e, which is used in Europe a lot. Its compound name is S-Adenosyl methionine, and in Italy it the top selling over-the-counter antidepressant. There have been 76 studies worldwide showing it has comparable efficacy to other anti-depressants, with less side effects. It is recommended to take 400-1600 mg a day. It is very expensive though. Read more on Depression and SAM-e.
Folic acid is another one. Low folic acid has been correlated with depression. The recommended dosage is 500 micrograms of folic acid a day. Read more about Depression and Folic Acid. Tryptophan is another natural remedy that is used, because it is a precursor to dopamine production. However, that can have sedative effects. Read more about Depression and Tryptophan.
For any of them, I suggest consulting your physician who has knowledge about how these remedies may interfere with other medications. I know that St. John’s Wort can interfere with HIV medications. Certain supplements can interfere with contraceptives. For obvious reasons, it is essential to consult professionals with any form of treatment you are undertaking for SAD and/or any other mental health disorder.
Click here to see FoundHealth’s 33 treatments for depression.
5 Responses to Dealing with Winter Depression: 6 Questions about Seasonal Affective Disorder
Leave a Reply to Amy Ahlfeld, Psy.D. Cancel reply
Your email address will not be published. Required fields are marked *
*
*
You may use these HTML tags and attributes: <a href="" title=""> <abbr title=""> <acronym title=""> <b> <blockquote cite=""> <cite> <code> <del datetime=""> <em> <i> <q cite=""> <strike> <strong>
Join Our Community
Archives
- January 2023
- December 2022
- September 2022
- August 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- March 2021
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
Subscribe
Sign up to receive FREE toolkit
From Dr. Hyman, #1 NY Times & Amazon Author
We never spam or sell your e-mail









Great review– thanks! However, here is a correction: Under Depression and Tryptophan, tryptophan is a precursor to serotonin, the calming, mood-elevating neurotransmitter, not dopamine, which enhances focus and motivation. I wrote about both extensively in Natural Highs.
A separate question was about vegans and depression: yes, B12 deficiency in vegans can certainly lead to depression and cognitive impairment too, since it’s needed to make essential neurotransmitters. THere may be insufficient protein in the diet as well. Just a caveat: vegans need to be extra careful to get all the nutrients they need.
Dr. Cass, Thanks for the correction. Yes- Tryptophan, an essential amino acid, increases the amount of serotonin in the brain when ends up increasing and fortifying these nerve circuits, which contributes to feelings of calm and well-being as well as relaxation and confidence.
I found this article really useful in distinguishing between SAD and depression, and the use of supplements and herbs to treat them.
More recently there does seem to be an increase in the number of women who I meet who are saying they feel down/depressed.
I would add Vitamin D deficiency especially when there is little sunlight, to the list of supplements and herbs. I have seen a number of amazing changes in some women’s emotions and happiness.
Vitamin D in people is lower in the winter, especially in areas that are overcast. Taking a supplement during this darker time of year often alleviates the depressive symptoms if they are seasonally brought on. I personally have experienced this. Studies on Vitamin D address this, as well.
Great article. I will use to help educate my patients who are dealing with depression/SAD. An additional thing to consider with regards to depression is the food/mind connection, particularly where food sensitivities are concerned. Prolonged IgG (type of immunoglobulin) immune response to foods can cause systemic inflammation at the cellular level which in turn can disrupt hormonal and neurotransmitter balance and activity, triggering or worsening anxiety, depression and even more severe conditions, such as ADD/ADHD, bipolar and schizophrenia. A common food sensitivity is gluten, however, even foods normally considered healthy, such as garlic or onions among many others, can trigger IgG response. Further, hormonal imbalance is integral to low thyroid function which is often implicated in depression and anxiety. If you suffer from depression, seasonal or otherwise, it may behoove you to investigate food sensitivity and thyroid dysfunction.