This week, FoundHealth sat down for an interview with Mark St. Peter, Therapeutic Physical Care Expert. As an expert on treating sciatica, we asked him about treatment options – from alternative approaches like acupuncture, to a discussion on surgery. Enjoy!
“There is a level of wellness beyond absence of symptoms that is only accessible through active pursuit of your own healing”
-Mark St. Peter, Dynamic Balance
Q: I think I might have sciatica. Who can treat me?
A: Conventional medicine options are physical therapy and chiropractic. If your condition is new, you should start by seeing an MD or DC (doctor of chiropractic). Both of these practitioners are “gatekeepers”, meaning that they can provide a diagnosis, refer you for imaging or to a specialist, and bill your insurance company.
Your physician will likely offer you:
1. Between 2-20 sessions of Physical Therapy
2. Bracing/splinting
3. Oral or injected anti- inflammatory medications
4. Painkillers
5. Surgery
Your chiropractor will offer you any combination of:
1. Corrective skeletal manipulation
2. Musculoskeletal work
3. Education
4. Perhaps elements of a physical therapy session.
*Both of these professions are governed by “standards of care”, but in reality the personality, experience and natural affinity will influence the nature of the services greatly.
*In chiropractic care, practices ranging from “adjustments” involving a swift aggressive twist or thrust, or a mild activator device to adjusting or balancing energy fields, depending on the individual practice.
With the information that you gather from their assessment and medical imagery you as a patient can begin to explore other treatment options.
There are many other “alternative” practices that are very effective at helping people overcome physical challenges like sciatica. Specialists in Feldenkrais, Pilates, physical therapy, and various other movement therapies can help people get over mild to moderate cases. Yoga can be and often is life changing. Massage therapy, acupuncture, and in some cases reflexology can be effective at restoring function. Then there are practitioners like myself who use mixed modalities. Ultimately long-term corrections will come from rebuilding your primal reflex pattern, which, in the case of sciatica, is centered around building strength and control in the lower lumber and pelvic areas. Keep in mind that if you want to avoid , or have already taken the medical route and are seeking alternatives there are many people practicing many crafts out in the world. You will likely have to try a few of them to find a fit you feel good about. Look for competence, some sort of track record, knowledge and respect for your condition and an you personally. Understanding that to overcome this difficulty requires a relationship, work and time.
Q: Is there a point at which there’s no turning back toward complete recovery? Or can I get better?
A: The only time sciatica is not reversible is if there is nerve damage or an impingement that can’t be repaired therapeutically or surgically. Most cases don’t involve nerve damage. When they do, it is because the sciatic impingement originates in the spine, where there are hard bony structures that can cause the nerve damage if misaligned, and it should go without saying, nerve damage can also be caused by trauma.
If you can achieve momentary relief using almost any intervention, that’s a good sign that it can get better. If, after a treatment, or in a specific position, you have a brief time of blissful comfort, I assert that that painless state can be made permanent.
Q: I exercise, am a healthy weight, use an ergonomic desk, try not to sit for too long at a time, and am healthy overall. Why did this happen to me?
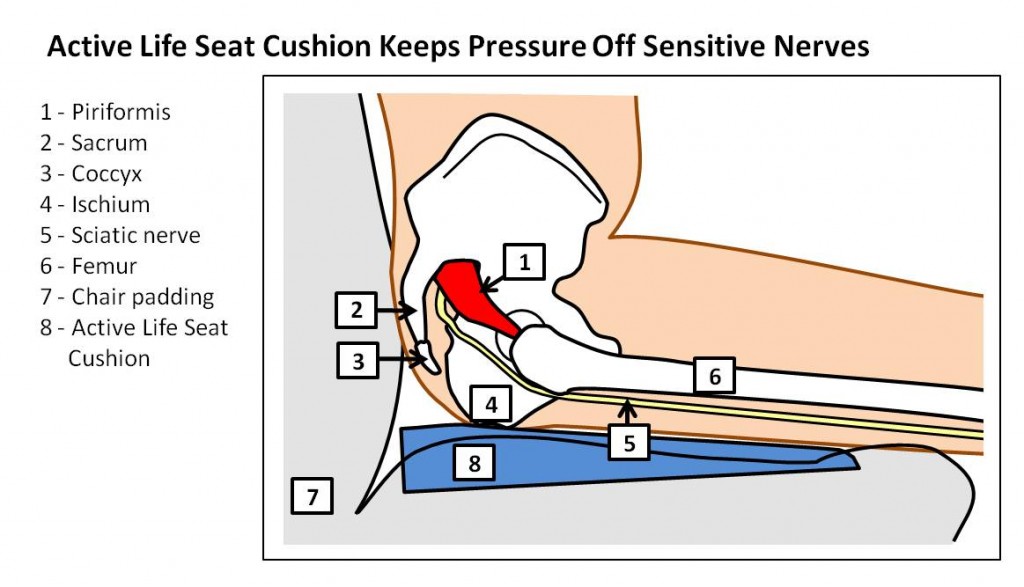
A: It’s a very distressing situation when we try to do everything right and we still suffer from discomfort. First, we need to examine some simple things in your life: Do you use a wallet and is it worn on the same side of the sciatica? If so, stop. Is there any history of back or hip injury or chronic pain? Next, we need to look at the seating in your life: your car seat, your desk chair and equipment, and your home furniture. You don’t want seating that compresses you from the side or rear. Deep cushy chairs that fold in on you and compress are not good. Firm chairs that tend to be more rounded in the center tend to be more comfortable and cause less irritation on the sciatic channel. Next we would look at your activities. What do you do for exercise? Are there any repetitive mechanical abnormalities? Running, a sport, or even attending knitting class regularly…there could be elements of any of those activities that might contribute.
It is likely that you will begin to see the origins of your condition after exploring these elements of your lifestyle, hobbies and activities. Has your doctor or other practitioner asked all these questions? If not, ask them to evaluate your lifestyle. See if you can find a practitioner who will give you a holistic lifestyle evaluation. Keep these things in mind when visiting various health professionals.
Q: Do I need surgery? Is there anything else I should try first?
A: Prior to any surgery, try everything and anything. There are many interventions for sciatica, some of which I mentioned. Sciatica is a condition that requires a personal commitment to overcome. Passive interventions will not allow you to completely regain function. It’s important to actively pursue causes and to implement corrective strategies. Surgery, though it may provide relief from the worst of symptoms, will rarely provide complete restoration of function on its own. Surgery is also fraught with risks. Suffice it to say the more significant the intervention, the greater the risks.
At the same time, surgical procedures, prosthetic devices, alternative strategies and medication advance constantly. With proper care you can quite often prevent the need for surgery.
Q: How long does recovering from surgery for sciatica take, and how can I speed up recovery?
A: Recovery from any surgical procedure generally requires anywhere from 6 weeks to 6 months for tissue healing alone. The more diligent you are with your program, the quicker and more complete the recovery will be. In the medical model, total recovery means being able to walk and work. I believe the absence of pain is not necessarily the best we can achieve. It is possible to teach people the value and methods of self care that improve quality of life after surgery, the same biomechanical patterns from before, left untreated, will likely continue. Surgery can fix things that are broken or worn, but surgery does not change the chronic biomechanical dysfunction that we all carry. Full recovery is dependent on rebuilding accurate kinetic patterns, so it’s dependent on using exercise or movement as part of your recovery plan.
Q: You mention both treatment and training as parts of overcoming sciatica. Can you explain the difference?
A: Treatment is anything that is done to you. It’s passively received. It could be bodywork, acupuncture, medication, ultrasound, electric stimulation, spiritual cleansings, hypnotherapy, injections or surgery…these are all passive treatments that are received. Training, on the other hand, is made up of the active things you do. This includes the habits you change and adapt, exercises that you learn, excuses that you unlearn, and the understanding that you gain through attempting to address your condition. Treatment can provide relief for the short term, while training maintains it for the long term. I can treat a condition repeatedly and get profound temporary relief. But as long as the underlying kinetic patterns exist, the problem will often recur. And it’s you engaging in the training part, in the reeducation part, that leads to long-term relief.
Q: Is there any day-to-day activity that might make my sciatica worse? How should I modify my day-to-day routine?
A: The #1 aggravator of sciatica is sitting. Remove wallets from pockets, and be aware of your furniture. Often car seats, in particular, tend to fold in on you. They have high sides and low middles. Sometimes putting a pillow in the bowl of the seat (possibly along with some lumbar support), or finding the right combination of support from underneath and behind, will prevent aggravation of the condition. In many cases, people will not feel the sciatic pain while they’re driving, but every time they drive their pain flares up afterward. There’s a mechanical irritation aspect to it, meaning that the tissues are irritated by mechanical forces within the body such as twists, turns, leans, or sitting in one place too long.
Q: Is chiropractic care safe for sciatica?
A: Generally yes. That said, not all chiropractors are the same. There are widely varying methods and techniques within the profession. It is important that whatever professional you see have experience with your condition, and be able to explain what the treatment program will look like before you engage. Avoid practitioners who are selling a guarantee or requiring an excessive long-term commitment. You should feel a tendency toward relief within the first 3-5 sessions, and you should gain insight to your condition as you continue to work with the individual. My personal preference is to work with chiropractic professionals who emphasize not only passive treatment, but kinetic retraining as well.
About Mark St. Peter: As founder of Dynamic Balance (www.dynamicbalance.com), Mark St. Peter developed the Therapeutic Physical Care™ approach to rehabilitation based on his own life experiences as a competitive athlete with two bachelors degrees (BS & BA), and a traumatic life-threatening, reality-altering injury. The subsequent journey from death’s door to therapeutic care specialist has informed his practice on every level.
With a 24-year career as a coach/trainer/therapist utilizing many healing arts and science traditions, Mark specializes in working with injury and chronic pain, helping clients overcome the barriers of disability and the emotional distress that accompanies limited physical function. Dynamic Balance clients cover the whole age spectrum and physical challenges including severe lateral sclerosis, chronic joint pain and replacement, athletes seeking a higher level of performance and physical functionality.
One Response to FH Interview Series: Learning to Cope with Sciatica
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
*
*
You may use these HTML tags and attributes: <a href="" title=""> <abbr title=""> <acronym title=""> <b> <blockquote cite=""> <cite> <code> <del datetime=""> <em> <i> <q cite=""> <strike> <strong>
Join Our Community
Archives
- January 2023
- December 2022
- September 2022
- August 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- March 2021
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
Subscribe
Sign up to receive FREE toolkit
From Dr. Hyman, #1 NY Times & Amazon Author
We never spam or sell your e-mail









Massage therapy can be also a good way to manage sciatica. Given proper attention to the key points in the body that needs to be massaged, it will soon be relieved